How to meet the new Medicaid work requirement: A state-by-state guide

Tada Images // Shutterstock
Medicaid is the public health insurance program that covers adults and children from low-income households as well as people of all ages with disabilities. There are 56 Medicaid programs and all are funded, in part, by the federal government. Each state, plus five U.S. territories, and Washington D.C., has its own Medicaid program.
Through the Affordable Care Act, 40 states and Washington D.C. have expanded Medicaid coverage. For these states, Medicaid includes people with higher incomes than previously qualified. Typically, expansion adults have incomes up to 138% of the federal poverty level (FPL).
The One Big Beautiful Bill Act of 2025 sets new work requirements for adults ages 19 to 64 living in states that have expanded Medicaid. The mandate is scheduled to begin by Jan. 1, 2027. (States can start the work requirements sooner.) The secretary of the U.S. Department of Health and Human Services can give states until Dec. 31, 2028, to begin.
Arkansas became the first state to implement Medicaid work requirements in 2018. By the time the short-lived program was shut down by a federal judge in 2019, about 18,000 people lost coverage (which was later restored). Nonexpansion states can also pursue Medicaid work requirements. Georgia has not expanded Medicaid, but it has had Medicaid work requirements since 2023. It is the only state with a waiver for this purpose.
More than 77 million people are covered by Medicaid and the Children’s Health Insurance Program (CHIP) as of September 2025. More than 40 million (52%) were adults. As of March 2025, at least 20 million adults covered by Medicaid are in the expansion group.
A 2023 KFF analysis of Medicaid-covered adults ages 19 to 64 found that most were working. And in a survey of health policy scholars, the majority said they don’t think work requirements will boost employment.
In this article, GoodRx, a platform for medication savings, explains Medicaid work requirements under the One Big Beautiful Bill Act.
Key takeaways:
- Medicaid work requirements for adults ages 19 to 64 among the Medicaid expansion population in 40 states and Washington D.C. are scheduled to begin Jan. 1, 2027. Georgia has had Medicaid work requirements since 2023 and is the only state with this mandate at the time of publication.
- To maintain Medicaid coverage, an “able-bodied” applicant or enrollee in the expansion population, who doesn’t qualify for an exemption, must complete at least 80 hours a month of combined work, community service, “work program” participation, and educational enrollment — or half-time educational enrollment alone.
- Health policy researchers and Congressional Budget Office analysts expect Medicaid work requirements to result in more than 5 million people losing insurance by 2034 and little, if any, increase in employment.
What are the new Medicaid work requirements in the One Big Beautiful Bill Act?
An “able-bodied” Medicaid enrollee subject to the Medicaid work requirements must complete one of the following every month:
- 80 hours of work, community service, and/or “work program” participation
- At least half-time educational enrollment
- 80 hours of combined work, community service, “work program” participation, and educational enrollment
States can also allow hardship exemptions. These include people who have been:
- Recently in the hospital
- Living in a county with a federally declared disaster or emergency
- Living in a county with a high unemployment rate
Your work status may be verified upon enrollment. In some states, this mandate will require up to three months of work when you apply for Medicaid. Your compliance will be checked during annual reenrollment and may be verified monthly.
Who is exempt from the new work requirements?
There are excluded individuals and mandatory exemptions. People who won’t need to meet the Medicaid work requirements are:
- Parents, guardians, and caregivers for children age 13 and younger or disabled individuals
- Pregnant women or individuals receiving postpartum Medicaid coverage
- Disabled veterans
- Current or former foster youth under age 26
- Medically frail individuals or those with special medical needs
- American Indians, Alaska Natives, and California Indians
- Participating in substance abuse treatment or rehabilitation programs
- Participants in work requirements for other benefits, such as Supplemental Nutrition Assistance Program (SNAP, or food stamps) or Temporary Assistance for Needy Families (TANF)
- Individuals who are incarcerated or who have been in the past three months
How do work requirements differ by state?
Georgia is the only state with an approved Medicaid work requirement waiver. Seven states have requests pending with the Centers for Medicare & Medicaid Services (CMS).
KFF is maintaining a Medicaid work requirements tracker, which has information about:
- States with approved work requirement waivers
- States with pending waiver requests that have been submitted to CMS for review
- Legislative action in progress or approved in states where Medicaid waivers must be affirmed by lawmakers before submission to CMS
This chart has details:
Medicaid work requirements approved and pending by state
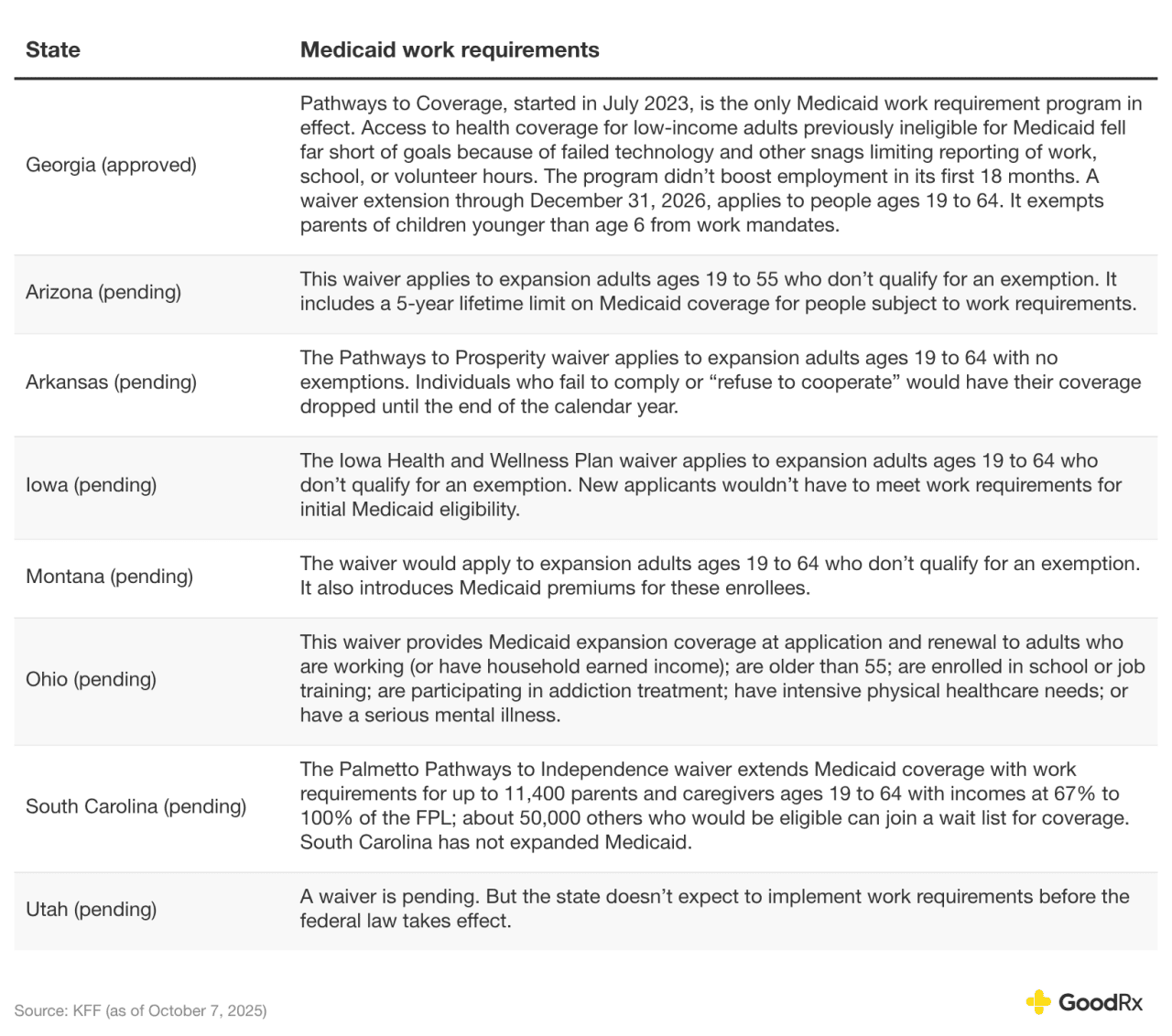
GoodRx
How often will the state verify your work hours?
Your compliance with work requirements may be verified when you sign up for Medicaid coverage. The application process could include a look-back period of one to three months. Work requirements will also be checked during annual renewal and at least every six months. Some states may verify work requirements monthly.
How Medicaid work requirements may affect your health insurance coverage
Congressional Budget Office analysts and health policy researchers have concluded that work requirements will lead to widespread insurance coverage losses for more than 5 million people by 2034. This will reduce access to care, including prescription medications. And in the survey of health policy scholars mentioned earlier, the majority believed most people subject to Medicaid work requirements would lose coverage due to challenges reporting hours — even if they were employed, volunteering, participating in job training, and/or going to school.
During the brief Arkansas program that started in 2018, more than 18,000 people lost their Medicaid. Coverage was restored, but the interruption left many with poorer health. Some continued with necessary care they couldn’t afford, which resulted in medical debt.
The bottom line
Medicaid work requirements for people ages 19 to 64 among the Medicaid expansion population in 40 states and Washington D.C. are scheduled to start by Jan. 1, 2027. Georgia, which has not expanded Medicaid, started a similar mandate in 2023. It is the only state with Medicaid work requirements in effect. Under the One Big Beautiful Bill Act of 2025, Medicaid enrollees in the expansion population who don’t qualify for an exemption must complete at least 80 hours monthly of combined work, community service, “work program” participation, and educational enrollment — or half-time educational enrollment — to keep their coverage. Health policy analysts and scholars predict nationwide Medicaid work requirements will cause insurance coverage losses for more than 5 million people by 2034 and won’t increase employment appreciably.
This story was produced by GoodRx and reviewed and distributed by Stacker.
![]()
